CERTIFIED MEDICAL CREDENTIALING SERVICES
Medical credentialing services are essential for healthcare providers who want to join insurance panels, maintain compliance, and ensure timely reimbursements. At MedStates, our top-tier provider enrollment and certified medical credentialing services assist solo practitioners, group practices, and clinics across the U.S. to deliver quality care without delays while we take note of securing and maintaining provider credentials. From CAQH and PECOS to commercial payer enrollment, our insurance credentialing experts steer through the complex landscape of insurance networks and regulatory requirements to maintain your credentials to keep your practice compliant, save time, minimizing delays, and reducing claim denials. Maintain your practice credibility with MedStates certified medical credentialing services and provider enrollment services!!!
CERTIFIED MEDICAL CREDENTIALING SERVICES
In the healthcare industry, medical insurance credentialing is one of the most important requirement to ensure the quality of care and the financial success of a healthcare practice. Whether you are a physician, part of a medical billing team, or work in administration of a healthcare practice, understanding insurance credentialing is a key to making sure that your practice stays compliant, remains profitable, and capable of billing insurance companies accurately.
What does it mean to be credentialed in healthcare, and why is credentialing and billing services so important in health industry. Let us explain what certified medical credentialing services are, why it is crucial for healthcare providers, and how it directly relates to MedStates comprehensive medical billing services.
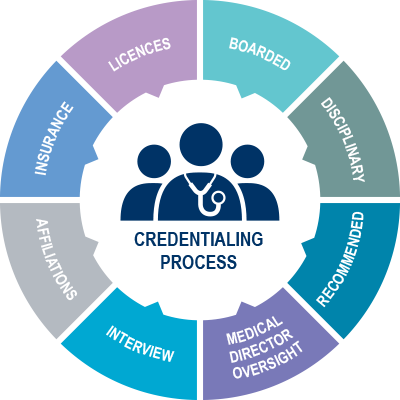
INSURANCE CREDENTIALING IN HEALTHCARE
Insurance credentialing in healthcare refers to the process of verifying a medical care provider’s qualifications, experience, and license to practice medicine to ensure that they are competent and legally authorized to provide medical care. When we talk about professional insurance credentialing, we refer to review of a provider’s:
- Relevant Professional Qualification
- Approved Certifications
- License to Practice Medicine
- Training and Residency
- Previous Practice History
- Insurance Malpractice Record
The enrollment and credentialing process with insurance ensures that providers meet the eligibility criteria for patient care, participate in insurance networks, and eligible to be reimbursed for medical services. So, when it is asked, “What does credentialing mean in healthcare?”. The answer is to ensure the safety, competence, and qualifications of a healthcare providers.


WHAT IS PROVIDER CREDENTIALING?
Since healthcare providers are at the forefront of patient care, the credentialing process for healthcare practitioners involves verifying a physician’s qualifications, training, malpractice history, and other essential details. These details determine their eligibility to practice medicine and bill insurance network for their services to insurance holders.
Physician credentials include not only educational history but also professional licenses and certifications that allow them to practice in certain specialties.
Provider credentialing is a requirement to get accepted into insurance networks. Without certified medical credentialing, providers cannot submit claims to insurance network, thus, leads to delay or rejection of claims.
Insurance credentialing is carried out usually by healthcare provider’s office or by a professional credentialing company hired by physicians that specializes in handling all the necessary documentation, submissions, and follow-ups with insurance companies.
MEDICAL CREDENTIALING CHECKLIST
AUTHORITIES FOR CREDENTIALING AND RE-CREDENTIALING
The insurance credentialing process for healthcare providers typically involves several key authorities and organizations that set standards and ensure compliance. These include:
- National Provider Identifier (NPI) Registry – Managed by the Centers for Medicare & Medicaid Services (CMS), the NPI Registry is an essential database for identifying healthcare providers. Every provider must obtain an NPI, which is used in billing and credentialing.
- The American Board of Medical Specialties (ABMS) – The ABMS certifies physicians in the United States in 24 different medical specialties and sub-specialties. Board certification is a critical part of the credentialing process for physicians. Insurance companies often require board certification from ABMS-accredited boards as part of their credentialing criteria.
- The Joint Commission (TJC) – The Joint Commission is a nationally recognized organization that accredits healthcare organizations and programs. It also plays a role in medical staff credentialing by ensuring healthcare facilities meet strict standards for patient care and safety.
- National Committee for Quality Assurance (NCQA) – The NCQA is responsible for accrediting healthcare organizations and also works closely with insurance companies to ensure providers meet high standards. It has specific standards for credentialing and recredentialing providers within health plans.
- State Medical Boards – Each state has its own medical board responsible for licensing and credentialing physicians within the state. These boards are responsible for verifying licensure and monitoring the credentialing process to ensure that doctors meet state-specific requirements to practice medicine.
- Council for Affordable Quality Healthcare (CAQH) – CAQH offers a centralized platform for healthcare providers to submit their credentialing information to multiple insurance companies and healthcare organizations. Many insurance companies require that providers complete credentialing through CAQH as part of the credentialing process for providers.
- Centers for Medicare & Medicaid Services (CMS) – For providers who wish to participate in the Medicare and Medicaid programs, CMS manages the Medicare Provider Enrollment, Chain, and Ownership System (PECOS), which is used to verify and enroll providers. CMS also plays a role in recredentialing providers for continued participation in these programs.
- Accreditation Association for Ambulatory Health Care (AAAHC) – For ambulatory care centers and outpatient clinics, the AAAHC is a leading authority for accreditation. They provide guidelines and credentialing requirements that healthcare organizations must meet to maintain quality standards.





HOW INSURANCE RELATES TO MEDICAL CREDENTIALING SERVICES?
In the context of medical billing, certified medical credentialing service ensures that the provider is eligible to submit claims to insurance network against approved insurance plan, for reimbursement. Insurance credentialing in medical billing directly impacts whether a provider will be reimbursed for services or his claims will be rejected. In some cases, when the credentials are not up-to-date, the payer companies may delay reimbursement of claims till submission of updated medical credentials.
MedStates certified medical credentialing services verify that the provider has met all the requirements to bill for services in compliance with insurance guidelines and state specific regulations. Without proper credentialing, the credentialing process for billing services can lead to denied claims, payment delays, and increased administrative costs. Moreover, when billing for a non-credentialed healthcare provider, MedStates medical billing experts has to go through intense payer requirements for clarification before recredentialing is done. This results in loss of time, efforts and positive energy. Yet, such claims often go to bad debts, claim denials as well as claim rejection.
Therefore, to ensure smooth medical billing services, MedStates ensure provider credentialing before submission of claims. This is why insurance credentialing and medical billing services often go side by side. When providers are properly credentialed, claims can be processed quickly, reducing the risk of financial disruption for healthcare practice as well as MedStates (since MedStates charge a percentage of paid claims as billing service fee), creating a win-win situation for medical service provider as well as our billing company.
How to Get Credentialed
A step-by-step guide for healthcare providers to complete insurance credentialing successfully
Step 1: Gather Required Documents
Collect your NPI, CAQH login, DEA certificate, license, malpractice insurance, CV, and W-9 form
Step 2: Complete Your CAQH Profile
Log in to CAQH ProView, fill out personal and practice information, upload documents, and attest your profile
Step 3: Submit Insurance Applications
Apply to Medicare, Medicaid, and commercial insurers like BCBS, Aetna, or UHC using PECOS or payer portals
Step 4: Follow Up & Monitor Status
Track your application progress, respond to payer requests, and document approval timelines for recredentialing
Step 5: Re-Attest and Stay Compliant
Re-attest your CAQH profile every 120 days and keep track of recredentialing requirements every 2–3 years
INSURANCE CREDENTIALING SERVICES - INDUSTRY EXPERTS
Who Needs Medical Credentialing Services?
Medical credentialing services are essential for any healthcare provider or organization that bills insurance companies or participates in payer networks. At MedStates, we work with a wide range of healthcare professionals and organizations, including:
Solo Providers
Independent physicians, therapists, or nurse practitioners starting private practice or switching states.Group Practices & Clinics
Multi-specialty or single-specialty practices needing credentialing for multiple providers and ensuring re-credentialing compliance.New Graduates & Recently Licensed Providers
We help you build your CAQH profile, NPI registration, and insurer applications from scratch.Behavioral Health Providers
Psychologists, counselors, and mental health providers navigating credentialing with Medicaid and commercial payers.Telemedicine
Virtual care providers needing multi-state credentialing and payer enrollment across geographic regions.Urgent Care & Ambulatory Clinics
High-volume centers requiring fast, accurate credentialing to keep operations smooth and reimbursement timely
For healthcare practitioners, medical credentialing is the process to ensure that their credentials are up-to-date and verified for enrollment with insurance network. Providers must undergo the health insurance credentialing to become eligible to provide patient care under various insurance plans. This allows the healthcare providers to submit claims for their services and receive payment in return.
For healthcare practitioners, joining hands with MedStates certified credentialing company for physicians can streamline the process. MedStates make sure that all insurance credentialing requirements are complied, applications are submitted correctly, and follow-ups with insurance companies are handled in a timely manner.
If you are looking for certified medical credentialing services, approved doctor credentialing services, or just need assistance with managing hospital credentials, it is important to find a trusted service like MedStates that understands the ins and outs of provider’s medical credentialing services and medical billing and coding service.
Not sure where to start?
Schedule a free consultation with a credentialing expert at MedStates and let’s build your roadmap to compliance and faster reimbursements.
Common Challenges in Medical Credentialing Services
Credentialing in healthcare is often more complex than providers anticipate. Some common challenges include:
Incomplete or outdated documentation (e.g., expired licenses or missing malpractice coverage)
Delays from payers due to processing backlogs or policy changes
Errors in CAQH or PECOS profiles
Lack of follow-up with insurance companies leading to credentialing expiration
Ineffective tracking systems resulting in missed re-credentialing deadlines
These issues can lead to serious consequences such as reimbursement delays, claim denials, and even removal from insurance panels.
Credentialing Denials & Revenue Impact
Data shows credentialing errors and delays can significantly harm practice finances:
- Over 54 % of medical practices report an increase in credentialing-related claim denials.
- Credentialing errors are responsible for up to 42 % of total claim denials in multi-provider groups.
- On average, fixing a denied claim costs:
– $25 per claim in physician practices
– $181 per claim in hospitals.
These issues delay reimbursement, strain cash flow, and drive up administrative costs.
Credentialing Timelines: What Providers Should Expect
| Type of Credentialing | Average Timeline |
|---|---|
| Initial Credentialing | 90–120 Days |
| Re-Credentialing | 60–90 Days |
| Medicare (PECOS) Enrollment | 45–90 Days |
| Medicaid Enrollment | Varies by State |
| CAQH Profile Verification | 7–14 Days |
Pro Tip: Begin the credentialing process at least 3–4 months before your planned start date with a new practice or payer.
Hidden Costs of Delayed Credentialing
Delayed payer onboarding and credentialing can result in significant lost revenue:
Nearly 46% of healthcare organizations report direct revenue impact from slow credentialing workflows.
A solo provider missing 900 visits over a 12-week credentialing delay could lose up to $83,500 in unrecoverable billing.
If a provider sees 20 patients per day at $100 average revenue, a single payer lapse could cost about $2,000 per day — or approximately $40,000 per month.
Pro Tip: Automating credentialing and constant monitoring can drastically reduce these losses.
How MedStates Streamlines Medical Credentialing Services
At MedStates, we don’t just submit paperwork—we provide end-to-end credentialing support to prevent costly delays and denials. Here’s how we set ourselves apart:
✅ Credentialing Audit: We review your CAQH, NPI, PECOS, and license statuses to ensure all data is accurate.
✅ Multi-Payer Expertise: Our specialists handle Medicare, Medicaid, and private insurers nationwide.
✅ Follow-Up Guarantee: We monitor applications weekly and maintain contact with all insurance panels.
✅ Re-Credentialing Alerts: You’ll receive reminders and support to maintain continuous enrollment.
✅ Transparent Reporting: Track your credentialing progress in real-time with our client dashboard.
Whether you’re a solo provider or part of a multi-specialty group, MedStates ensures credentialing doesn’t disrupt your revenue cycle. As a leading medical credentialing company for physicians, we manage the provider credentialing process to ensure that your practice remains eligible for timely and accurate reimbursements for the healthcare services rendered. Whether you are looking for medical credentialing services, or need assistance with medical billing services, MedStates one-stop RCM solutions help with everything from provider enrollment to patient eligibility verification, medical coding and billing solutions, claim submission, denial management and accounts receivable follow-up services.
Moreover, MedStates assist in financial and business consultancy services which includes practice management, business expansion, bookkeeping services, financial reporting, dashboard creation and financial management.
Case Study: Faster Credentialing for a Multi-Specialty Clinic
A multi-specialty outpatient clinic in Ohio with 18 providers, struggled with frequent delays in credentialing new providers with major commercial insurers. Their in-house administrative team lacked the capacity to manage re-credentialing and follow-ups effectively, resulting in recurring claim denials and significant disruptions to their revenue cycle.
The clinic faced consistent delays in getting new providers credentialed with top commercial insurers. Their in-house admin team lacked bandwidth to track re-credentialing and follow-up timelines, causing claim denials and revenue disruption.
MedStates Solution:
We took over the full credentialing and enrollment process, including:
- Complete audit and update of all provider CAQH and NPI profiles
- Direct communication with payers like BCBS, UHC, Cigna, and Medicare
- Setup of automated reminders for re-credentialing
- Transparent progress tracking via MedStates dashboard
Results (within 3 months):
- Credentialing approval time reduced by 42%
- Eliminated $18,700/month in claim denials due to enrollment gaps
- Re-credentialing compliance improved to 100%
- Clinic administrator reported a 60% reduction in credentialing workload
