
The Essentials OF Medical Billing and Coding IN Modernized Healthcare Revenue Cycle Management
In the healthcare industry, the secretarial work of medical billing, administration and coding is the prerequisite on which revenue cycle management (RCM) depends. This vast process comprises everything from patient registration to insurance claims processing and ensures that healthcare providers are reimbursed accurately and timely for the services they render. But going through the specific details of medical billing and coding can be overwhelming for the healthcare professionals due to its lengthy documentation that cost them time.
While reading this page, you will get clear understanding of fundamentals of medical billing and coding, the process of medical billing and coding and the steps needed to optimize revenue cycle management of a medical practice. From the basics of medical coding systems to the complexities of insurance claim denials and subsequent appeals, we will help you learn the best practices
The Importance of accuracy in Medical Billing and Coding
Accurate medical billing and coding are critical components in the healthcare system, serving as the bridge between patient care and financial reimbursement. When healthcare providers deliver services, it is essential that these services are correctly documented and coded to ensure that they receive exact and accurate compensation from insurance companies and patients in some cases. Errors in medical billing and coding leads to significant financial losses, delayed payments, claim denials and even legal repercussions. Therefore, the integrity of the billing process is paramount for the sustainability of healthcare practices.

Moreover, accurate medical billing and coding also serves as a tool to increase patient satisfaction and gain more trust. Patients expect transparency and clarity regarding their healthcare expenses. When billing statements are accurate and easy to understand, it fosters a sense of confidence in the healthcare provider. Conversely, inconsistent or erroneous bills can lead to confusion, dissatisfaction, and even disputes over charges. This relationship between billing accuracy and patient trust highlights the necessity for healthcare providers to prioritize effective billing practices.

Additionally, accurate medical billing and coding play a vital role in health data management and analytics. The data collected through billing processes contribute to broader healthcare trends, insurance analytics, and regulatory compliance. Proper coding ensures that healthcare providers can report statistics accurately, which can influence public health policy and funding decisions. Thus, the importance of precision in medical billing and coding extends beyond individual practices; it affects the healthcare landscape as a whole.
Key Terms and Concepts in Medical Billing and Coding
Navigating the realm of medical billing and coding requires familiarity with specific terminology and concepts that serve as the foundation of the process.
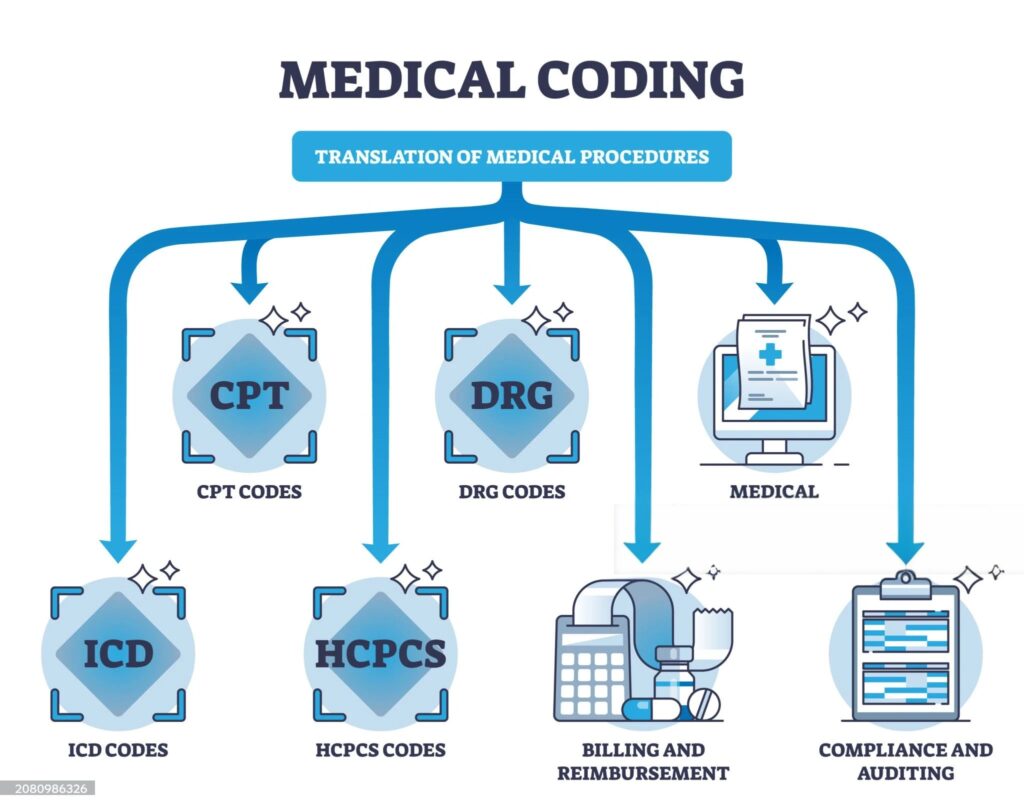
- One of the most fundamental terms is "CPT," which stands for Current Procedural Terminology. This coding system is used to describe medical, surgical, and diagnostic services and is essential for billing purposes. Each procedure or service is assigned a unique CPT code, ensuring clarity in what was performed during a patient visit.
- Another critical concept is the "ICD" code, which refers to the International Classification of Diseases. These codes are used to classify and code diagnoses, symptoms, and procedures. Understanding the different versions of ICD, such as ICD-10, is vital for accurate coding. The transition from ICD-9 to ICD-10 introduced a more comprehensive coding structure, allowing for greater specificity in patient diagnoses and enhancing the potential for accurate reimbursement.
- Lastly, understanding "EOB" or Explanation of Benefits is crucial for both providers and patients. An EOB is a statement from an insurance company that outlines what services were covered, the amount billed, and the amount the patient is responsible for paying. This document is essential for patients to understand their financial responsibility and for providers to reconcile payments. Familiarity with these key terms enables stakeholders in healthcare to communicate effectively and navigate the billing process with greater ease.
PROCESS OF Medical Billing and Coding FOR HEALTHCARE PRACTICE
- The medical billing and coding process begins at the point of patient registration, where demographic and insurance information is collected. This initial step is crucial as it sets the stage for the subsequent coding and billing activities. Accurate patient information ensures that claims can be processed without delays or errors. Healthcare providers must verify insurance coverage and eligibility to determine the patient’s benefits and potential out-of-pocket costs.
- Once the patient has received care, the next phase involves translating the services provided into specific codes. Medical coders review the documentation from healthcare providers, which includes patient history, examination notes, and treatment plans. They then assign the appropriate CPT and ICD codes to each service rendered. This step requires a keen eye for detail and a thorough understanding of coding guidelines, as each code must accurately reflect the services performed and the patient’s diagnosis.
- After coding is complete, the billing process begins. Medical billers compile the coded information into claims, which are submitted to insurance payers for reimbursement. This step often involves communication with insurance companies to ensure claims are processed smoothly. If a claim is denied, understanding the reason behind the denial is crucial for resubmission or appeal. Thus, the medical billing and coding process is a cycle of meticulous documentation, coding accuracy, and effective communication, all aimed at maximizing revenue for healthcare providers.
Common Challenges in Healthcare RCM
Healthcare revenue management is fraught with challenges that can impede the efficiency of medical billing and coding processes.
One of the most common issues faced is claim denials. Denials can occur for various reasons, including incorrect coding, lack of documentation, or discrepancies in patient information. When claims are denied, it not only affects cash flow for healthcare providers but also requires additional time and resources to resolve the issues, leading to increased administrative burdens.
Another challenge is the complexity of insurance policies and reimbursement rates. Each insurance provider has its own rules regarding coverage, which can change frequently. This variability means that healthcare providers must stay updated on the latest regulations and guidelines to ensure compliance and optimize reimbursement. Understanding the nuances of different payer contracts and maintaining accurate financial records can be daunting, especially for smaller practices with limited resources.
Additionally, the increasing prevalence of healthcare fraud poses a significant challenge to revenue management. Fraudulent activities can lead to substantial financial losses and legal complications for healthcare providers. To mitigate these risks, it is essential for practices to implement robust compliance programs and conduct regular audits of billing and coding processes. By proactively addressing these challenges, healthcare organizations can enhance their revenue management strategies and maintain financial health.
Best Practices TO BRING EFFICIENCY in Billing & Coding
Implementing best practices in medical billing and coding is essential for enhancing efficiency and accuracy in revenue management.
One of the foundational practices is ensuring thorough documentation by healthcare providers. Accurate and detailed clinical notes are critical for coders to assign the correct codes. Providers should be trained on the importance of comprehensive documentation, which not only supports billing but also improves patient care.
Another key practice is regular training for coders and billers. The healthcare landscape is constantly evolving, with changes in coding guidelines, regulatory requirements, and payer policies. Continuous education ensures that medical billing and coding professionals remain knowledgeable about the latest updates, reducing the risk of errors and improving overall compliance. Regular workshops, webinars, and access to online learning resources can greatly benefit coding and billing teams.
Furthermore, leveraging technology can significantly enhance the efficiency of medical billing and coding processes. Utilizing electronic health record (EHR) systems with integrated billing solutions can streamline the documentation and coding workflows. Automated coding tools can assist in minimizing human error, while data analytics can provide insights into billing patterns and claim denials. By embracing technology, healthcare organizations can optimize their revenue cycle management and focus on delivering quality patient care.
TechnologICAL Solutions for Revenue CYCLE Management (RCM)
In the digital age, technology plays a pivotal role in streamlining healthcare revenue management.
- One of the most significant advancements is the adoption of electronic health records (EHRs). EHR systems allow for the seamless documentation of patient encounters, making it easier for healthcare providers to capture and code services accurately. With integrated billing functionalities, EHRs facilitate real-time data sharing between clinical and billing departments, reducing the risk of errors and improving the overall efficiency of revenue management.
- Another noteworthy technology solution is the implementation of revenue cycle management (RCM) software. RCM systems automate various aspects of the billing process, from appointment scheduling to claims submission and tracking. These systems help healthcare providers monitor their financial performance, identify trends in claim denials, and streamline workflows. Moreover, RCM solutions often come with analytics features that enable organizations to assess their revenue cycle performance and make data-driven decisions to enhance efficiency.
- Additionally, telehealth technology has emerged as a game-changer in healthcare revenue management. The rise of telehealth services has necessitated updates in coding and billing practices to accommodate virtual visits. Leveraging telehealth platforms that integrate with billing systems ensures that providers can accurately code and bill for remote services. As telehealth becomes increasingly prevalent, staying updated on coding changes related to virtual care is essential for maintaining revenue integrity.


IMPORTANCE OF TRAINING, DEVELOPMENT AND CERTIFICATIONS IN Billing and medical Coding
Training and certification are critical components for anyone looking to succeed in the field of medical billing and coding.



- Various organizations offer certifications, such as the Certified Professional Coder (CPC) from the American Academy of Professional Coders (AAPC) and the Certified Coding Specialist (CCS) from the American Health Information Management Association (AHIMA). These certifications validate the knowledge and skills necessary for accurate coding, billing, and compliance in healthcare settings. Obtaining certification not only enhances job prospects but also ensures a deeper understanding of coding guidelines and regulations.
- In addition to certification programs, ongoing education is essential for professionals in this field. The healthcare landscape is ever-evolving, with frequent updates to coding systems, regulations, and technology. Participating in workshops, webinars, and online courses can help coders and billers stay informed about industry changes. Many professional organizations offer resources for continuing education, allowing individuals to earn credits while enhancing their skills and knowledge.
- Moreover, hands-on experience is invaluable for those pursuing a career in medical billing and coding. Internships or entry-level positions in medical offices, hospitals, or billing companies provide practical experience that complements formal training. This experience not only helps individuals apply their knowledge in real-world scenarios but also builds a professional network that can lead to future job opportunities. Investing time in training and gaining practical experience is crucial for anyone seeking to excel in this field.
Outsourcing OF Medical Billing and Coding Services
- Outsourcing medical billing and coding services has become an increasingly popular option for healthcare providers seeking to enhance their revenue management processes. One of the primary advantages of outsourcing is cost-effectiveness. By partnering with MedStates Medical Billing Services, healthcare practices can reduce overhead costs associated with maintaining an in-house billing department. This allows providers to allocate resources more effectively, focusing on patient care rather than administrative tasks.
- Another significant benefit of outsourcing is access to expertise and advanced technology. Medical billing companies employ professionals who are trained and experienced to cope up with difficulties in coding and billing industry. These experts are up-to-date on the latest regulations, coding changes, and industry best practices, which can lead to improved accuracy and reduced claim denials. Additionally, outsourcing partners often utilize sophisticated software solutions that streamlines medical billing processes and enhance reporting capabilities, providing valuable insights to address performance gaps.
- However, outsourcing is not without its challenges. Effective communication between healthcare providers and billing companies is crucial for successful collaboration. Providers must ensure that the outsourced team understands their specific needs and workflows to prevent any disruptions in the billing process. Establishing clear lines of communication and setting expectations can help mitigate potential issues and create a productive partnership that creates a win-win situation for healthcare provider and medical billing company.

MEDSTATES: The Future of Medical Billing SERVICES
The future of medical billing and coding is poised for transformation as the healthcare industry continues to evolve. To stay compliant and growing with the healthcare industry, MedStates has started adapting emerging technologies, such as artificial intelligence which is playing a significant role in streamlining medical coding processes and improving billing accuracy. These advancements promise to reduce the administrative burden on healthcare providers, allowing them to focus more on patient care while we enhance their revenue cycle management (RCM). In addition to technological advancements, MedStates Medical Billing Services is prepared to shape the landscape of medical billing and coding. As healthcare policies change, MedStates medical billing professionals are ready to adapt new coding standards and reimbursement models. MedStates is committed to adapting change and continuous learning & training for ensuring compliance and optimizing revenue streams in an ever-changing environment.

