How EHR in Mental Health Is Transforming Behavioral Health Care
BLOG OUTLINE
- The role of electronic health records in revolutionizing mental healthcare
- Key benefits of EHR in mental health treatment
- Core EHR features tailored for mental health providers
- How EHR in mental health improves care coordination
- EHR in mental health for patient engagement and communication
- Leveraging EHR in mental health for data and analytics
- Overcoming challenges in Implementing EHRs in mental healthcare settings
- Best practices for maximizing EHR in Mental Health settings
- The future of EHRs in revolutionizing mental healthcare
- Conclusion: EHR in mental health is shaping the future of behavioral care
The Role of Electronic Health Records in Revolutionizing Mental Healthcare
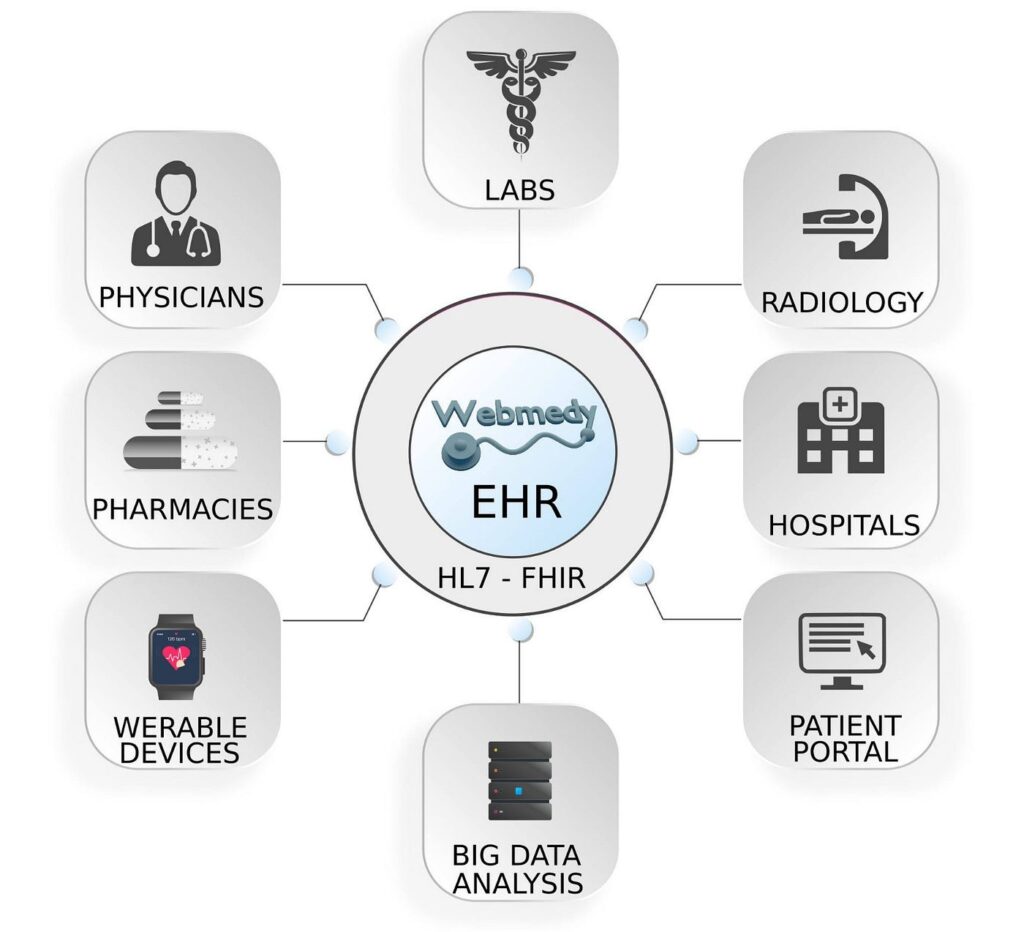
The field of mental healthcare is undergoing a profound digital transformation, driven by the widespread adoption of Electronic Health Records (EHRs). These dynamic systems allow mental health professionals to efficiently access, update, and share comprehensive patient data—including medical histories, psychiatric evaluations, medication records, and therapy notes—in real time and with robust privacy controls. EHR in mental health not only enhances clinical accuracy and treatment effectiveness but also reduces the administrative burden on providers.
Furthermore, EHRs improve communication between interdisciplinary care teams, support evidence-based treatment planning through data analytics, and empower patients to take an active role in their mental health journey. With integrated features like telehealth, automated alerts, and patient portals, EHR in mental health is reshaping the delivery of behavioral care to be more personalized, collaborative, and outcome-driven.
This article explores how EHR in mental health is revolutionizing every aspect of mental healthcare—from provider workflows and patient engagement to analytics, compliance, and the future of care innovation.
For Insurance Credentialing, Medical Billing Services and other services
Key Benefits of EHR in Mental Health Treatment
The integration of electronic health records (EHRs) into mental healthcare systems offers numerous advantages that significantly enhance the overall quality of care.
One of the most notable benefits is the streamlined access to comprehensive patient information. Mental health professionals can easily retrieve a patient’s medical history, treatment plans, and medication records without sifting through stacks of paperwork. This not only saves time but also minimizes the risk of errors associated with manual documentation. By having all pertinent information at their fingertips, clinicians can make more informed decisions, leading to improved patient outcomes.
EHRs also improve documentation and billing processes, which are often cumbersome in mental healthcare. With electronic records, clinicians can efficiently document sessions and treatment plans, leading to better compliance with regulatory requirements. The billing process becomes more transparent and systematic, reducing the likelihood of billing errors. This efficiency not only benefits providers but also translates into a smoother experience for patients, who can focus on their recovery rather than administrative hurdles.
EHRs also contribute to enhanced communication between healthcare providers. Mental health often requires collaborative care involving various specialists, such as psychiatrists, psychologists, and social workers. EHR systems facilitate seamless sharing of patient data among these professionals, promoting a cohesive approach to treatment. This interconnectivity reduces the chances of duplicative testing, conflicting medications, and miscommunication, ensuring that all members of the care team are on the same page. As a result, patients receive more coordinated and effective care tailored to their specific needs.
Overall, the advantages of EHRs in mental healthcare represent a significant leap towards a more efficient, effective, and patient-centered model of care.
For Insurance Credentialing, Medical Billing Services and other services
Core EHR Features Tailored for Mental Health Providers
EHR systems built for mental healthcare include features that address the unique needs of behavioral health providers. These include:
Customized templates for documenting psychotherapy sessions, psychiatric evaluations, and risk assessments.
Integrated screening tools (e.g., PHQ-9, GAD-7) for conditions like depression, anxiety, PTSD, and substance use disorders.
Outcome tracking dashboards to monitor patient progress and adjust treatment plans accordingly.
Telehealth integration, supporting secure video consultations and virtual documentation.
Real-time alerts for medication interactions or suicidal ideation risk flags.
These specialized features enhance the efficiency and clinical value of EHR in mental health, benefiting psychiatry and therapy practices alike.
One of the key features is the ability to document behavioral health assessments and treatment modalities. These systems often include templates tailored for mental health evaluations, making it easier for clinicians to conduct thorough assessments and record findings accurately. This specificity helps ensure that all relevant aspects of a patient’s mental health are captured, allowing for better tracking of progress over time.
Another important feature of EHRs in mental healthcare is the integration of standardized screening tools and outcome measures. Many EHR systems allow providers to incorporate evidence-based assessments directly into their workflows. This facilitates routine screening for conditions such as depression, anxiety, and substance use disorders. By regularly utilizing these tools, clinicians can monitor symptoms and treatment efficacy, enabling timely adjustments to care plans and improving overall patient outcomes. The incorporation of outcome measures also supports accountability and quality improvement initiatives within mental healthcare settings.
Additionally, EHR systems often include functionalities for telehealth, which has become increasingly important in the wake of the COVID-19 pandemic. The ability to conduct virtual appointments within the EHR framework ensures that mental health providers can maintain continuity of care while accommodating patient preferences. This feature also allows for remote monitoring of patients, enhancing follow-up care and ensuring that individuals receive the support they need, regardless of geographical barriers. The integration of telehealth capabilities into EHR systems further underscores their role in transforming mental healthcare delivery.
How EHR in Mental Health Improves Care Coordination
Effective mental healthcare often requires coordination across multiple providers and care settings. EHR in mental health facilitates this by:
Centralizing patient data, including behavioral and physical health information.
Enabling real-time updates across hospitals, outpatient clinics, and community health centers.
Preventing medication errors or conflicting treatment plans by synchronizing care workflows.
Supporting case management tools that track referrals, follow-up appointments, and care transitions.
For patients with co-occurring disorders (e.g., diabetes and depression), this level of coordination ensures providers treat the patient thoroughly rather than isolated symptoms. EHR systems in mental health enable more integrated care across diverse medical environments.
EHR in Mental Health for Patient Engagement and Communication
Patient engagement is a cornerstone of successful mental health treatment. Modern EHR systems support this through:
- Secure patient portals, giving individuals access to their mental health records, therapy notes, medications, and care plans.
- Two-way messaging between patients and providers—reducing communication delays and supporting ongoing care outside sessions.
- Appointment reminders and educational content, empowering patients to stay informed and proactive about their health.
- Support for remote access, which is especially useful for individuals with anxiety or mobility issues who may avoid in-person visits.
This patient-centered approach enhances trust, accountability, and treatment adherence.
PATIENT PORTALS
One of the standout features of modern EHR systems is the incorporation of patient portals. These secure platforms enable patients to access their health information, including treatment plans, medication lists, and upcoming appointments. By empowering patients with this information, EHRs foster a sense of ownership over their health and encourage proactive participation in their treatment.
DIRECT COMMUNICATION
Furthermore, patient portals often include messaging capabilities that allow for direct communication between patients and their mental health providers. This feature enhances accessibility, as patients can ask questions, seek clarification on treatment, or provide updates on their condition without needing to schedule an in-person visit. This convenience can be particularly beneficial for individuals with anxiety or other mental health concerns that may make face-to-face communication challenging. By facilitating ongoing dialogue, EHRs help to build stronger therapeutic alliances between patients and providers.
EDUCATIONAL RESOURCES
Educational resources are another vital aspect of patient engagement that EHRs can support. Many systems offer access to information about mental health conditions, treatment options, and self-care strategies. By providing patients with relevant educational materials, EHRs can support informed decision-making and equip individuals with the knowledge they need to navigate their treatment journey.
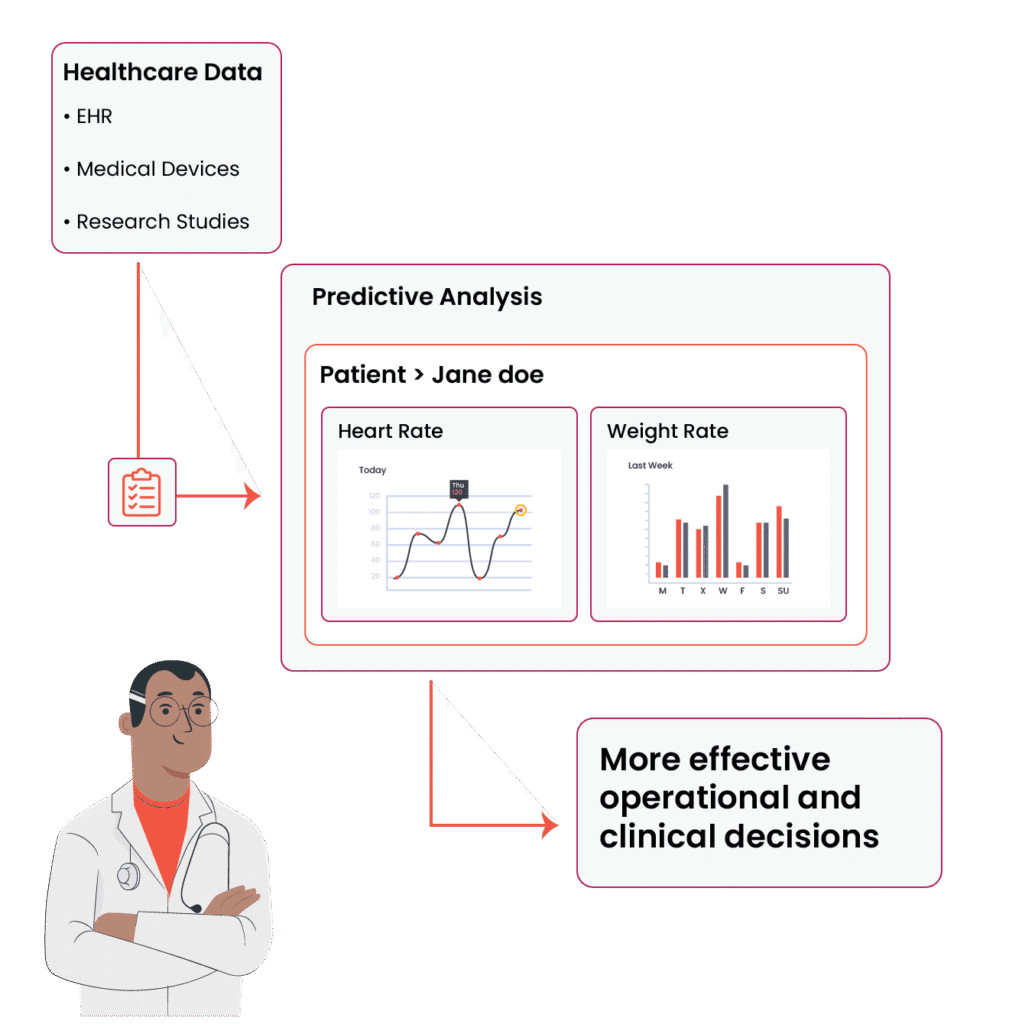
Leveraging EHR in Mental Health for Data and Analytics
Data analytics represents a transformative opportunity for mental healthcare, and EHRs serve as a powerful tool for harnessing the potential of patient data. By collecting and analyzing large datasets, mental health providers can identify trends, assess treatment efficacy, and evaluate the overall quality of care. For example, analyzing data on patient demographics, treatment modalities, and outcomes can reveal patterns that inform best practices in mental health treatment. This evidence-based approach allows providers to refine their interventions and improve patient care.
Additionally, EHRs facilitate the identification of at-risk populations through predictive analytics. By leveraging historical data, mental health providers can develop models that identify individuals who may benefit from early interventions or targeted outreach. For instance, analytics can flag patients with a history of substance use who may be at risk for relapse, prompting proactive engagement by their care teams. This proactive approach not only helps in addressing mental health issues before they escalate but also contributes to more efficient allocation of resources within the healthcare system.
Furthermore, the integration of data analytics into EHRs supports continuous quality improvement initiatives. Mental health organizations can use aggregated data to assess performance metrics, track progress toward organizational goals, and identify areas for enhancement.
Overcoming challenges in implementing EHRs in mental healthcare settings
Despite the advantages, EHR adoption in mental healthcare presents unique challenges:
Cost barriers: Smaller clinics may struggle with the upfront investment required for system installation and training.
Learning curves: Clinicians unaccustomed to digital platforms may experience disruptions in workflow.
Privacy concerns: Mental health records are highly sensitive, requiring strict adherence to HIPAA and 42 CFR Part 2 regulations.
Data entry fatigue: Without proper templates and automation, clinicians may face documentation burnout.
Solutions include selecting behavioral health-specific EHR vendors, allocating resources for ongoing training, and involving clinical staff in the customization and rollout process.
Best Practices for Maximizing EHR in Mental Health Settings
To fully leverage EHR systems in mental healthcare, providers should adopt these best practices:
Customize documentation workflows: Tailor templates for evaluations, therapy notes, and progress tracking to match your practice model.
Train and retrain staff: Ongoing education helps staff adapt to new tools, updates, and compliance changes.
Engage patients: Encourage portal use, invite patient feedback, and involve them in goal-setting.
Utilize analytics dashboards: Regularly review outcomes, treatment metrics, and care gaps to improve service delivery.
Implement telehealth workflows: Seamlessly integrate virtual care into your EHR system for broader access.
These practices enhance both clinician productivity and patient satisfaction.
The future of EHRs in mental healthcare looks promising, with ongoing advancements in technology and a growing emphasis on patient-centered care. As artificial intelligence and machine learning technologies continue to evolve, EHR systems are expected to incorporate predictive analytics and decision support tools that further enhance clinical decision-making. For example, AI algorithms may analyze patient data to suggest personalized treatment plans or flag potential risks based on historical patterns. These innovations have the potential to revolutionize how mental health providers approach diagnosis and treatment.
Moreover, the integration of interoperability standards will play a crucial role in the future of EHRs. As different healthcare systems increasingly share data, mental health providers will benefit from a more comprehensive view of a patient’s overall health. Interoperability allows for seamless transitions of care, ensuring that mental health providers have access to vital information from primary care and specialty providers. This holistic perspective will enhance the coordination of care and improve outcomes for patients with complex health needs.
Telehealth is also poised to continue its expansion alongside EHR systems. As more mental health providers adopt virtual care models, the integration of telehealth functionalities within EHRs will become increasingly important. This will not only facilitate ongoing communication between providers and patients but also support remote monitoring and follow-up care. The synergy between EHRs and telehealth will create a more flexible and accessible mental healthcare landscape, ultimately leading to improved patient experiences and outcomes.
Conclusion: EHR in Mental Health Is Shaping the Future of Behavioral Care
EHR in mental health has emerged as a transformative force in behavioral and psychiatric care. It enhances care coordination, fosters data-driven decision-making, supports secure communication, and empowers both providers and patients.
While implementation challenges remain, the long-term benefits of adopting EHR systems customized for mental health far outweigh the initial hurdles. As AI, telehealth, and interoperability evolve, EHR in mental health will continue to redefine how mental health services are delivered. Its strategic use not only supports efficiency but also strengthens patient-centered outcomes.
The future of mental healthcare is bright, and EHRs will undoubtedly play a pivotal role in this transformation. As we continue to explore the possibilities of data-driven care, personalized treatment approaches, and integrated healthcare systems, the role of electronic health records will remain central to enhancing the quality of mental health services and improving the lives of individuals facing mental health challenges.
Ready to modernize your mental health practice? Contact us today to learn how our tailored EHR solutions can help you streamline care, improve outcomes, and stay ahead in a rapidly evolving healthcare landscape.


